Beyond Symptoms: How to Measure Real Progress When You’re Living with Parkinson’s
The word “progress” conjures images of forward momentum and recovery. But for people living with chronic conditions like Parkinson’s, progress can sometimes mean the continuation, or even worsening of symptoms. And this can lead to emotional frustration, confusion, and even discouragement.
So, how we define and frame progress matters deeply. The language we use affects not only how we think about our condition but also how we approach treatment, track changes, and make decisions. Rather than allowing “progress” to be a one-sided word, we can redefine it to include every meaningful step, even the small ones.
For those navigating Parkinson’s, the core challenge is not just managing symptoms. It’s understanding how to measure improvement meaningfully and using that knowledge to drive better outcomes.
Recognizing the Warning Signs
Many individuals struggle with unclear metrics around whether they are getting better or worse. In fact, even small declines can feel like major setbacks when there’s no broader context to understand them. And this ambiguity can lead to fear, frustration, or disengagement from treatment.
A few common experiences highlight this issue:
Unclear metrics of improvement: Many people struggle to determine whether they’re actually improving or maintaining status.
Emotional fatigue: Repeated assessments can feel burdensome or demoralizing, especially if the results seem to suggest decline.
Communication gaps: Without clear tracking tools, patients and providers may not be aligned on how symptoms are affecting daily life.
Invisibility of certain symptoms: Mood, sleep, fatigue, and other non-motor symptoms are often underreported and undetected.
Some symptoms, especially non-motor ones like mood or sleep disturbances, are often missed during typical assessments. Without tools to measure what really matters in daily life, people feel unheard or unsupported. When patients and providers aren’t aligned, meaningful communication and decision-making suffer.
Reclaiming Your Strength: A Plan for Progress
Living with Parkinson’s can make progress feel out of reach, especially when every day looks a little different. But progress is possible, and often it starts with better clarity, not just more effort.
By understanding your symptoms and tracking your function, you can begin to take control. With the right tools and support, you can reclaim your strength, step by step, on your terms.
I. Tracking with Purpose
For those living with Parkinson’s, the decision to track symptoms is a personal one. Some may prefer to focus on healthy habits and enjoy daily life without the additional burden of measurements, and that choice is completely valid. But for others, tracking can offer valuable insights. Rather than serving as a reminder of decline, it can become a supportive tool that guides decisions and highlights what’s working.
Tracking progress helps reveal patterns, monitor changes, and identify when adjustments might be needed, whether in treatment, exercise routines, or lifestyle habits. Having clear data fosters a sense of control and encourages proactive action, rather than resignation. Many individuals have maintained or even improved their strength, independence, and quality of life through consistent assessment. When used thoughtfully, tracking becomes less about diagnosis and more about empowerment.
II. Using established tools: MDS-UPDRS
The MDS-UPDRS (Movement Disorder Society-Unified Parkinson’s Disease Rating Scale) is a tool designed to assess and track symptoms in people with Parkinson’s disease. It was created to enhance the original UPDRS by offering more accuracy and consistency in measurement. Today, it’s widely used in both medical care and research around the world.
III. A closer look at the MDS-UPDRS Score Sheet
The MDS-UPDRS (Movement Disorder Society-Unified Parkinson’s Disease Rating Scale) is a standardized score sheet used by neurologists to track the progression of Parkinson’s disease. It’s divided into four distinct sections, each designed to assess a different aspect of the condition:
Part I - Non-motor symptoms: cognitive changes, hallucinations, mood issues, sleep problems, and autonomic symptoms like constipation or dizziness.
Part II - Motor experiences in daily life: daily living, including speech, eating, dressing, and mobility.
Part III - Motor examination: tremors, rigidity, balance.
Part IV - Motor complications: dyskinesias, and when medication isn’t working effectively (“off” times).
While not all clinics use this tool consistently, it’s valuable to ask your neurologist, “Are you using the MDS-UPDRS to track my symptoms?”. Being informed about your score can lead to earlier interventions and better outcomes.
IV. Using the Score and Communicating with Your Doctor
Scores may go up or down for different reasons - medication changes, injuries, or activity levels. A higher score doesn’t automatically mean your Parkinson’s is getting worse. What matters is how the score aligns with your experience and whether symptoms are bothersome to you.
Talk openly with your neurologist about the UPDRS. Ask if they use it and let them know if you’d like to know your score. You might say, “I want to be proactive in managing my Parkinson’s, and this information helps me understand what’s changing.”
V. The Value of Functional Assessments
There are a few important notes about these assessments. First, there are many different tests that can be done, whether you’re working individually with a physical therapist or attending group classes that include some form of assessment. Each test has a different purpose, and we choose them based on the individual’s needs and goals.
It’s also important to understand that in these cases, we’re not directly measuring Parkinson’s symptoms. Instead, we’re assessing function - things like balance and mobility. Parkinson’s disease does play a role, but it’s just one part of the bigger picture.
VI. Beyond Symptoms: Functional Assessment That Supports Daily Life
In addition to age norms, some tests include cutoff scores that signal fall risk. For instance, completing a task slower than a set time can suggest an increased likelihood of falling. This helps us proactively target areas of concern.
We also track individual progress over time by repeating assessments every six months. This helps us identify improvements, stability, or areas of decline. That early detection is key to adjusting programs and maintaining function.
Here are a few examples of what we’ve seen in practice:
Sit-to-Rise Test
This measures the ability to get down to and up from the floor without using hands or knees. It reflects core strength and full-body mobility. One client improved from needing two hands and a knee to only using one hand - clear evidence of enhanced functional strength.
Grip Strength & Nine-Hole Peg Test
These assess fine motor control and upper-body strength. While one client remained below age norms in peg test speed, her performance was stable over time, an important indicator of maintained function, which is itself a form of progress.
Trail Making Test
This evaluates cognitive flexibility. One client showed a 15-second improvement in Trail B, reflecting improved processing speed and cognitive coordination. These results exceeded age norms - a significant win.
360° Turn Test & Single-Leg Balance
One client improved dramatically on single-leg balance, jumping from 4 to 9 seconds to 20 seconds on both legs - far above the age norm of around 11 seconds. Her 360° Turn Test showed smoother, faster turning as well.
Walking Performance
Although walking speed decreased slightly, the client adopted a wider step strategy to help prevent freezing. Slower doesn’t always mean worse; in this case, it was a conscious adaptation to maintain safety and stability.
These results, when viewed together, tell a fuller story. Some areas improved, others held steady, and a few need more attention. But overall, the direction was positive and actionable.
Tracking Progress: A Holistic Approach to Parkinson’s Care and Improvement
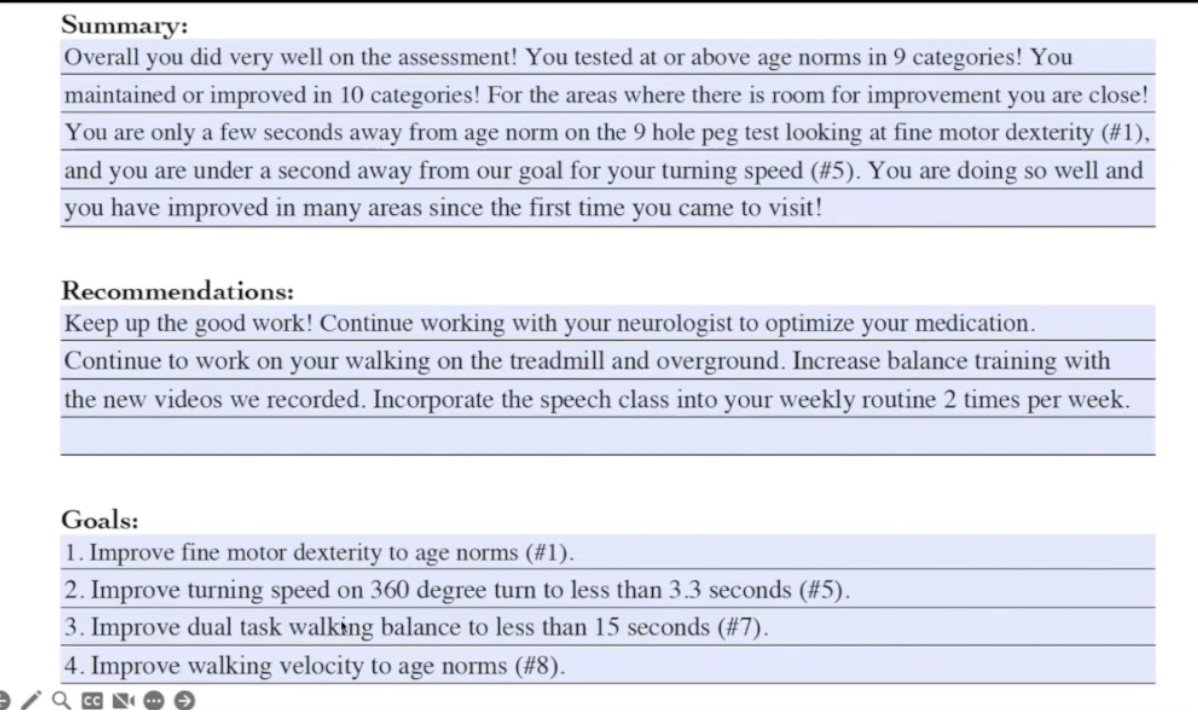
Following the client’s recent assessment, we documented a summary, recommendations, and specific goals. She met or exceeded age norms in nine categories and came very close in several others, showing significant improvement since her first evaluation. She’s doing great overall, though some areas - like fine motor dexterity, dual-task walking, and balance - still offer room for refinement.
We’re continuing to work with her neurologist to optimize medication, and an interesting finding emerged: she actually experienced more freezing on medication than off. To address this, we introduced new balance training strategies, which she plans to incorporate into her routine. For the six-minute walk test, we wisely conducted the assessments on two separate days to avoid fatigue-related performance issues and ensure more accurate results.
VII. Incorporating Subjective Experience: Pro-PD
The Pro-PD (Patient-Reported Outcomes in Parkinson’s Disease) is a self-assessment designed to capture how Parkinson’s affects your daily life. Unlike clinical evaluation, it allows individuals to measure their own symptoms without needing a therapist or doctor. It’s a continuous, patient-centered tool that reflects symptom severity and quality-of-life impact.
Traditional tools like the UPDRS focus on clinician-observed physical symptoms. In contrast, the Pro-PD was developed to spotlight the symptoms most meaningful to people actually living with Parkinson’s. It can be done at home, uses a “lower is better” scoring scale, and helps track changes over time.
Why it matters:
Gives patients a voice
Highlights symptoms that may not show up during physical exams.
Reveals trends in subjective well-being
It captures crucial aspects of daily life, like fatigue, pain, and sleep quality, that often go unmeasured in clinical tests.
Supports better communication with care teams
This makes it a valuable communication tool for both patients and healthcare providers.
Tracking these subjective symptoms can reveal patterns or changes that objective tests might miss. It also provides context to help explain why someone’s functional abilities may fluctuate. In this way, the Pro-PD helps create a fuller, more personalized understanding of Parkinson’s.
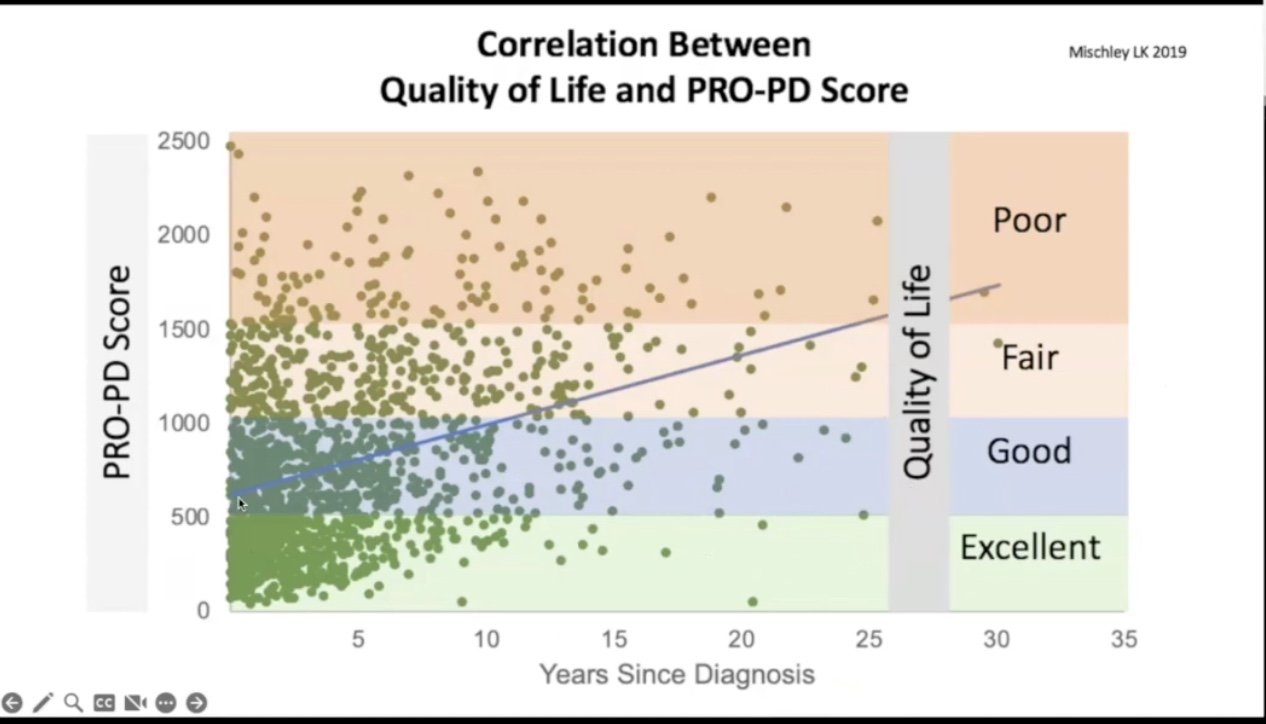
VIII. Why Frequency and Intensity of Exercise Matter in Parkinson’s Progression
Dr. Laurie Mischley’s MVP (Modifiable Variables in Parkinson’s) study is uncovering powerful insights into how lifestyle choices affect Parkinson’s disease progression. Through biannual surveys and the use of the PRO-PD (Patient-Related Outcomes in Parkinson’s Disease) scale, researchers are identifying strong correlations between daily habits and long-term outcomes. One standout finding is that people who exercise daily have PRO-PD scores an average of 300 points better than those who don’t, equating to a nine-year difference in symptom progression.
This kind of data is helping answer key questions that most studies overlook, especially around exercise frequency and intensity. Dr. Mischley’s findings show that consistent, frequent exercise - ideally three to seven days per week - significantly slows symptom advancement, with each additional day providing greater benefit. High-intensity activities like running appear particularly effective, and although weight plays a role, the overarching trend is clear: the more often and more vigorously people with Parkinson’s exercise, the better their outcomes.
IX. Tracking Progress and Staying Ahead
Dr. Laurie Mischley created the Pro-PD based on the belief that Parkinson’s progression can be influenced, and even improved, with the right approach. But to identify what works, we need consistent measurement. The Pro-PD helps track changes over time, empowering people to take ownership of their progress.
It’s also a credible tool, correlating well with established scales like the PDQ-39, PROMIS, and UPDRS. At diagnosis, the average Pro-PD score is just over 500, and the typical progression rate is about 38 points per year. But that rate isn’t guaranteed. Many people stay well below the curve, and some even improve with focused interventions.
X. Accessible Tools for Tracking
While physical assessments are easiest to perform in person with a therapist or fitness professional, online options are also available for members. For remote sessions, written instructions are provided beforehand, and some tests, like the six-minute walk, are completed independently before the virtual meeting. Other assessments can be done together over Zoom, followed by a discussion to interpret the results.
Many of these tests can also be done independently at home with some initial guidance. Having simple equipment and a partner to help with timing can make the process smoother and more accurate. Whether conducted in person, virtually, or on your own, these assessments offer valuable insights into your current abilities and areas for improvement.
a. ProPD.org
The PRO-PD tool helps you track changes over time, which is especially useful when trying new routines or treatments. For instance, if you change your diet or start a new exercise plan, you can compare your scores after a few weeks or months. There’s no limit to how often you use it - just choose what feels most helpful to you.
It can also improve communication with your care team, including your spouse or healthcare providers. Comparing perspectives may reveal important details you hadn’t noticed on your own.
You can complete the PRO-PD online at propd.org, right from your computer. It’s a simple process that can offer valuable insight into how your symptoms are evolving over time. Several individuals have used the tool consistently and found it helpful in tracking both improvements and setbacks.
b. Parkinson’s Symptom Tracker App
Besides the website, there’s a free app called Parkinson’s Symptom Tracker that you can download. After creating an account, you’ll be guided to enter your basic info and start tracking symptoms across specific timeframes. The more consistently you use it, the more useful your data becomes.
The tool calculates a total symptom score and shows a graph of your results over time. It includes 35 symptoms - like walking, drooling, constipation, and daytime sleepiness - that you rate on a scale from “no problem” to “severe”. At the end, it highlights your most bothersome symptoms and presents them in a list or chart view.
Functional Progress through Therapist-Led Assessments
We each have unique life experiences, genetics, and levels of activity that contribute to how we show up in these assessments. That’s why Parkinson’s is only part of the history - it’s not the whole story. These assessments are focused on your ability to do the things you want and need to do every day.
That’s also why therapist-led assessments feel more relevant to real life. They go beyond symptoms and look at how those symptoms impact your actual abilities. This functional focus helps identify both strengths and opportunities for growth.
Join us: Support Beyond Symptoms
In-person Exercise Classes
At Rogue Physical Therapy and Wellness, we specialize in providing a comprehensive program designed for individuals with Parkinson’s. We offer 40 classes a week across six different types of exercise, catering to five levels of intensity to meet the unique needs of each individual.
Our approach goes beyond just exercise. We provide ongoing support from physical therapists who are available to answer questions, offer guidance, and ensure you stay on track with your wellness journey. With a focus on holistic care, we are committed to helping you manage Parkinson’s and improve your quality of life through continuous support and exercise.
If you’re in the Orange County, California area, we invite you to check out our in-person classes at Rogue Physical Therapy and Wellness. Join us in person here for expert-led training that supports long-term success.
Online Access for Global Reach
Can’t join in person? No problem. Our online membership at Rogue in Motion, launched in 2020, allows participation from anywhere. Remote assessments, live Zoom sessions, and self-guided options ensure you get the same expertise and support.
Using the code FREEMONTH, you can enjoy your first month free, along with a 7-day free trial to explore coaching, expert guidance, and exercise resources.
Here’s a snapshot of what you’ll have access to:
Cardio Classes
Boxing at Home
Functional Strength + Skill-Based Training
Mind-Body & Recovery
Speech Classes (2x/week)
Cooking Class (Weekly)
Community Meetings
Whether we’re working together in person or online, the goal is the same - to support you every step of the way and help you thrive. Let’s redefine progress, not just as fewer symptoms, but more strength, clarity, and joy in your daily life.
Conclusion: Redefining Progress on Your Terms
Tracking Parkinson’s doesn’t have to be clinical, cold, or discouraging. When used with purpose, it becomes a compass - showing you what’s working, what’s improving, and where to focus your efforts.
Whether through the MDS-UPDRS, functional assessments, or self-report tools like Pro-PD, you’re gathering puzzle pieces to form a clearer picture of your health. Combine that with expert support, intentional movement, and a strong community, and you’ve got a powerful strategy for living well with Parkinson’s.